Guiding Principle II: Discussion and rationale
This article explores some observations and science that may support the idea that myofascial pain and the sensation of ‘stiffness’ are curiously connected.
My second guiding principle that I use every day in the assessment and treatment of chronic pain is the idea that myofascial referred pain patterns can present as ‘stiffness’. In other words, when a patient describes stiffness in a certain location at the end of their range of movement, rather than manipulate the location of the stiffness I will manipulate the location of trigger points that can refer ‘pain’ to that location. This single concept has revolutionised my approach to assessment and treatment. Now, whenever I treat and assess range of movement, I pay attention to the exact location of the patient’s stiffness and my first palpatory assessment is searching trigger point locations that can refer ‘pain’ to the vicinity that the patient is describing their stiffness as emerging from. Rather than palpating the muscles in the vicinity of the stiffness itself. This raises all sorts of questions…
Is pain, pain?
Is the subtle ‘painless’ restriction caused by Travell and Simons’ ‘taut band’ in the muscle fibres or is it caused by the overlying fascia?
There is one thing that is for sure: this notion rattles and confuses our concept of trigger points and myofascial pain.
Let’s tease it out . . .
Excuse the pun.
The work of Travell et al. has always revolved around ‘pain’. The myofascial pattern is ‘pain’. The trigger point is a painfully sensitive nodule within a taut band. This nodule is described literally as contracted muscle fibres. In other words, Travell et al. have gone straight to the mechanical. To quote:
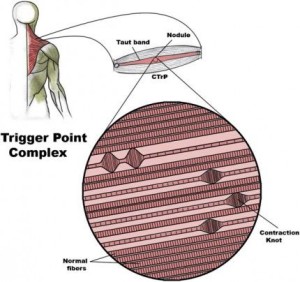
‘…we now know, based on histopathology, that a palpable nodule and an associated taut band are essential features of a myofascial TrP…’ (1)
The research in the Trigger Point Manuals delves heavily into the mechanical components of myofascial pain referencing the electrodiagnostic evidence which has measured a low-grade ‘noise’, or electrical activity in the trigger point location. This occurs though the rest of the same muscle is electrically silent. This observation suggests some interaction between the trigger point fibres and the autonomic nervous system.
Secondly Travell et al. reference the research on macro effects on muscle fibres around the trigger point vicinity (2). Multiple studies have observed the structural features of contraction knots amongst normal muscle fibres. These chronically contracted fibres seem well explained by the ‘Energy Crisis Theory’ (3). Travell et al. propose an integrated hypothesis that incorporates research from both of these areas of research.
It stands to reason then that when muscle fibres are shortened, range of movement will be reduced – resulting in stiffness! So stiffness is surely just due to the mechanically tight muscle fibres.
Sounds simple, right?
I think there is more to it . . .
I am going to suggest that that mechanically shortened muscle fibres and the electrical activity and chemical responses associated are the effect, not the cause. I am not questioning the electrical autonomic nervous component and the chemical/mechanical observations that Travell et al. have cited. It seems clear that all these effects are very real. What I am proposing is that the fascia around or throughout the muscle body – and even between the muscle fibres themselves – may create the initial, subtle stiffness or restriction in movement. Then when the fascia has ‘modelled’ the skeletal muscle in this way for some time, the end result is mechanically contracted muscle fibres as described by Travell et al. in their description of a trigger point.
I am suggesting this purely as a result of anecdotal clinical observation. What I observe clinically is the presence of stiffness that is not yet described by the patient as ‘pain’. Yet that stiffness corresponds to the myofascial pain pattern observed by Travell et al. and resolves when the trigger point location that is capable of referring ‘pain’ to that area is manipulated.
Myofascial force transmission . . .
More recent research has caused us to rethink totally our primitive notions of how muscles work.
We typically assume that the power of a muscle is generated purely by the contraction of muscle fibres that run the length of the muscle and are attached to the bone via tendon at either end. This notion is now outdated.
We now know that the active part of the muscle fibre – the sarcomere – is attached not only to the next sarcomere in parallel but also the collagenous (tendon-type) fibres along the full length of the muscle. This means that as a muscle contracts it pulls on the tendon at either end AND the endomysium; that is the ‘skin’ of the muscle. Then this muscle skin is connected to the skin of adjacent muscles. This is called myofascial force transmission. In other words:
‘In real bodies, muscles hardly ever transmit their full force directly via tendons into the skeleton, as it is usually suggested by our textbook drawings. They rather distribute a large portion of their contractile or tensional forces onto fascial sheets!’ (4)
Cells appear to modulate the tonicity and architecture of fascial tissues . . .
There is growing number of research papers that suggest that that fascia itself can actually move of its own accord. That it can contract and model posture and limit movement. Perhaps it can even cause ‘stiffness’ all by itself.
In a 1993 examination of human lumbar fascia by Yahia et al., a group of biomechanical investigators discovered its ability for tissue contraction. Three years later, the German anatomy professor, Staubesand, in an examination of the lower leg, documented the presence of smooth muscle like cells in the fascia (5). Upon this background Schleip, Jager and Klingler have done more recent research regarding cells in the fascia and their ability to affect posture and movement. They titled their paper ‘Fascia is able to contract in a smooth muscle-like manner and thereby influence musculoskeletal mechanics.’ (6)
So what?
As I have mentioned in previous articles, I am quietly confident that when we manipulate the soft tissues we primarily stimulate the fascia. I believe that by successfully manipulating the fascia we can ‘remodel’ posture and movement. I suspect that the ‘stiffness’ a patient feels at the end of their range of movement is mediated by the fascia and is a precursor to the full blown mechanically contracted muscle fibres described as trigger points.
Why is this important?
Firstly it is important because it opens the door to suggest that a trigger point may not be a trigger point. That this whole mechanism is more complicated. We have, for the sake of this training, stuck to the conventional trigger point terminology.
Secondly, this is important because although your patients ‘pain’ may be due to an obvious trigger point, the movement patterns in the five secondary muscles that are not referring pain need to be assessed and treated in order to restore full function to that region. Dysfunction in these secondary muscles will only present as ‘stiffness’ yet this is the same mechanism as the ‘painful’ muscle just in a less advanced form. It is still dysfunction.
Observations from the treatment room . . .
Typically, my patients get improvement 24-48 hours after treatment. In some cases five days later! If fascia does indeed contract and move in a smooth muscle-like way, and if we can indeed manipulate it to respond and remodel then it makes sense to me that change would occur a day or two after treatment.
Another observation: In my palpation I have found tension or restriction to often be regional. Although I search for myofascial restrictions in specific muscles, there is normally clusters of trigger points or restrictions in groups of muscles with similar functions. This may suggest that sheets of fascia have a lot more to do with where trigger points develop than strain to individual muscles. This would be consistent with the idea that muscles transfer a large portion of their contractile forces through fascial sheets, not just bone to bone, but one muscle to the next.
In short . . .
You will notice by all the ‘I believe’ and ‘I think’ statements that what I am talking about in this article really is an ongoing discussion.
I sure am excited about where the science is going though! It is intriguing.
References
-
Travell et al: Myofascial pain and Dysfunction – The Trigger Point Manual. Vol 1. Upper half of the Body. Second Edition. Lippincott Williams & Wilkins, USA 1999
-
Simons DG, Hong CZ, Simons LS: Presence of electrically active loci in human trigger points, endplate zones, and active taut bands. (In press)
-
Mense S, Simons DG: Muscle Pain. Williams & Wilkins, Baltimore. (In press)
-
Schleip R, Findley TW, Chaitow L, Huijing PA: Fascia – The Tensional Network of the Human Body. Churchill Livingstone, New York, 2012
-
Schleip R, Jager H, Klingler W: Fascia – The Tensional Network of the Human Body. Churchill Livingstone, New York, 2012 (p. 158)
-
Schleip R, Klingler W, Lehmann-Horn F. Published in Liepsch D: Proceedings of the 5th World Congress of Biomechanics. Munich, Germany, 2006 (p. 51-54)












Leave a Reply
Want to join the discussion?Feel free to contribute!