Peroneal proprioception – Be the guru on ankle stability
 Myotherapy is not only about pain relief. It is about function. The chronic instability left in ankles for years after an acute plantar flexion inversion injury is a classic case of myofascial dysfunction with no pain. And it is ridiculously easy to get amazing results with what you know. Be the guru on ankle stability.
Myotherapy is not only about pain relief. It is about function. The chronic instability left in ankles for years after an acute plantar flexion inversion injury is a classic case of myofascial dysfunction with no pain. And it is ridiculously easy to get amazing results with what you know. Be the guru on ankle stability.
*Note: This post is written for professionals, so may be more technical than others.
Plantar flexion Inversion.
The classic ankle injury.
As we know this injury typically occurs when an athlete lands on an opponent’s foot or when an older person simply misjudges the ground under them.
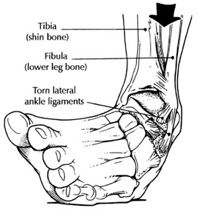 If done badly the ankle will swell and turn black and blue and generally takes 6-12 weeks to recover. Typically the lateral ligaments of the ankle are injured. Primarily the ATFL (anterior talofibular) then the CFL (calcaneofibular) and to a lesser extent the PTFL (posterior talofibular). In the majority of cases these ligaments are sprained at grade 1 or 2 and if you’re really unlucky grade 3 – complete rupture.
If done badly the ankle will swell and turn black and blue and generally takes 6-12 weeks to recover. Typically the lateral ligaments of the ankle are injured. Primarily the ATFL (anterior talofibular) then the CFL (calcaneofibular) and to a lesser extent the PTFL (posterior talofibular). In the majority of cases these ligaments are sprained at grade 1 or 2 and if you’re really unlucky grade 3 – complete rupture.
Now conservative rehabilitation of this injury is RICE in the first 48 hours, followed by crutches if needed, then weight bearing with assistance of strapping, then strengthening exercises, proprioceptive training (standing on one foot, wobble board and so on) and return to sport or normal activity.
It never really got better.
How many times have you heard this?
Months or years later a patient with a history of ankle injury will describe their ankle as ‘weak’.
They continue with sport, have little or no pain, but find they cannot play without the ankle strapped. In some cases they will describe that the ankle wants to swell a little after exercise or they will indicate pain under or around the lateral malleolus. All of this is written off as ‘normal’ ever since they rolled or injured that ankle months or years ago. It simply has never been the same . . .
In unfit individuals I have seen many examples where weakness is so apparent that the person will roll the ankle, or fall, as the ankle ‘gives way’ on a daily basis. Stepping on something as subtle as a pebble can cause the ankle to ‘let go’.
Magic.
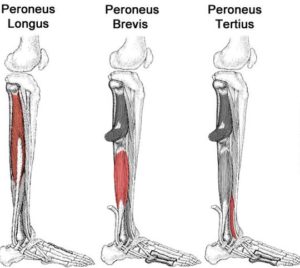
In my experience to date, every time a patient has described these symptoms I have been able to identify and resolve Myofascial restrictions (TrPs) in one or all of their peroneal muscles.
You may be saying: ‘Big deal. That is obvious.’
What is fascinating however is when the peroneal muscles are carefully investigated and manipulated, just how spontaneously the proprioception is restored. The right manipulation on the peroneals for literally a couple of minutes has led repeatedly and consistently to:
- a massive increase in proprioception
- a reduction or elimination of pain
- a reduction or elimination of swelling
It’s like magic.
The improvement is so dramatic, that in cases where there is no ligament rupture present, even with injuries that are years old, I have encouraged athletes after just one treatment to begin to reduce how often they strap the ankle.
Note this: There was no stretching involved. No strength work. No wobble board. And the improvement is immediate. I have treated acute injuries inside the first six weeks of rehab in the same way, with careful manipulation of the peroneal muscles even as the swelling is apparent and weight bearing is only just being resumed. Such treatment will give pain relief and a greater sense of stability.
In many long-term cases after only a treatment or two, the chronic ankle instability is resolved! It is not unusual for me to mention to the same patient years later, ‘How is that ankle?’ and they will say, ‘I have never rolled it again.’
What is happening?
As Myotherapists we all know that trigger points (or Myofascial restrictions) refer pain. But it is rarely as obvious, as in the case of ankle injury, just to what extent TrPs affect proprioception. What we observe when these peroneal TrPs are resolved effectively, seems to be the resolution of a deliberate inbuilt mechanism of the body that refers pain, restricts movement, ‘dumbs down’ proprioception and reduces strength. What I am referring to is the trigger point mechanism. For more on this read my Guiding Principle I and the accompanying discussion.
Think about it. All of the symptoms I have mentioned are traditionally treated separately and with various means.
- For the pain – anti-inflammatories, pain killers, steroidal injections and so on.
- For the proprioception and strength – strength and coordination exercises to ‘build up’ the weak muscles.
- For the range of movement – stretching and massage.
Yet a simple skilful manipulation can gain all of these benefits in seconds. The power we have in our hands as Myotherapists is extraordinary.
What is happening physiologically?
Clearly TrPs are established in the peroneal muscles either during the injury event, or else established in some compensatory way in the days and weeks to follow.
Did you know?
That fascia is gaining recognition as our ‘most important perceptual organ’ (1). Langevin stated, ‘It is likely that the connective tissue continuum of fasciae and fascial structures serves as a body-wide mechanosensitive signalling system with an integrating function analogous to that of the nervous system.’ (2) The truth of this concept may be no more obvious than in the case of the peroneal myofascial complex.
The myriad of tiny unmyelinated proprioceptive and free nerve endings are found almost everywhere in the fascial tissues providing proprioception and very likely nociception (pain feedback). Immediately underneath the skin, epidermis and dermis is an enveloping layer of dense and areolar connective tissue and fat called the ‘superficial fascia’. Marwan Abu-Hijleh et. al (3) explain that not only does this subcutaneous tissue (fascia) connect the skin to the underlying deep, dense fascia which invest muscles and aponeurosis throughout the body, but other scientists explain that this layer seems to be endowed with an exceptionally rich density of proprioceptive nerve endings (4). In other words, science is beginning to suggest that the ‘thinking’, highly responsive fascia is literally just under the skin.
These ideas would indicate that not only is the peroneal myofascial complex a ‘thinking’ structure but stimulating proprioceptive improvement may occur but just manipulating the skin and muscle.
Check out ‘Guiding Principle I: Chronic pain an intelligent messenger’ for more discussion on this.
What does my treatment look like?
Personally, I typically work through clothing or a sheet, I always use a cross-fibre form of manipulation and my manipulation is brief. In this scenario I would firstly survey by palpation the lower limb. I would be paying particular attention to all three of the peroneal muscles: peroneus longus, brevis and tertius. I encourage you to study the locations in these muscles where Travell indicates TrPs may occur (5).
I would also survey by palpation soleus, tibialis anterior and posterior, flexor and extensor hallucis longus.
 When I am surveying muscle by palpation I am searching the areas where I know that Myofascial restrictions (TrPs) can occur.
When I am surveying muscle by palpation I am searching the areas where I know that Myofascial restrictions (TrPs) can occur.
I perform firm, slow cross fibre manipulation as a form of survey, assessment and treatment. After searching all the muscles listed above I note any that contain localised Myofascial restriction. I then return and manipulate each site for perhaps 20 seconds in the same way. (For more on slow, firm cross-fibre manipulation, check out my Guiding Principle III.) I will work around the affected sites sequentially spending a little time (20 seconds) on each. I have found that manipulating then leaving a site of Myofascial restriction gets better results than manipulating for a long time in one location.
Now this is where it gets subjective. I revisit each site and see if it feels different to the previous manipulation. So I am assessing and treating. Always assessing and treating at the same time. I am sure we all have a different sense of feel, but I can tell when a change has occurred and the TrP or Myofascial restriction has resolved.
Once I am confident that the TrPs have resolved, I ask the patient to weight bear and walk normally and see how they feel. I will encourage them to use the foot normally. I will then ask them to pay careful attention to symptoms during the week.
In the scenario where the symptom is painless weakness, improvement may only be apparent after the patient has experienced multiple weeks without actually rolling the ankle, or experienced an episode where it would have previously given way.
Conclusion.
Of course further proprioceptive conditioning with the use of a wobble board is well worthwhile, especially in the case of athletic competition where performance is paramount. But for the average Joe, no such training is normally required. He is generally ‘over the moon’ with the improvement.
It seems clear from my clinical experience that TrPs don’t simply cause pain but retard proprioception. This is really obvious in the case of the peroneal muscles, but if you consider this truth in relation to TrPs or Myofascial restrictions elsewhere like in the back, neck or knee for example, then the implications for assessment and treatment are huge.
You can be the guru on ankle stability.
– Tim
PS. I am developing workshops to teach my technique so if you are keen to learn a faster, more effective way to treat and gain some PD then send me an email to register your interest and I will let you know when they are on.
Finally, sign up to receive my articles as I write them and feel free to ‘Like’ King Myotherapy on Facebook.
References:
-
Schleip R, Findley TW, Chaitow L, Huijing PA. Fascia – The Tensional Network of the Human Body. Churchill Livingstone, New York, 2012 (p. 77)
-
Langevin H, Yandow, J. Connective tissue: A body-wide signalling network? Med. Hypotheses [Internet]. 2006 Feb 17; 66 (6): 1074-7. PubMed PMID: 16483726
-
Abu-Hijleh MR, Roshier AL, Al-Shboul Q, et al. 2006. The membranous layer of superficial fascia:evidence for its widespread distribution in the body. Surg. Radiol. Anat. 28, 606-619.
-
Tesarz J, Hoheisel U, Wiedenhoefer B, et al. 2011. Sensory innervation of the thoracolumbar fascia in rats and humans. Neuroscience 194, 302-308.
-
Travell et al. Myofascial pain and Dysfunction – The Trigger Point Manual. Vol 2. The Lower Extremities. Lippincott Williams & Wilkins, USA 1983 (p. 371-396)










Leave a Reply
Want to join the discussion?Feel free to contribute!